Abstract
Introduction: Acquired von Willebrand disease (VWD) is uncommonly observed in patients with Waldenström Macroglobulinemia (WM), and necessitates treatment intervention. The clinical characteristics for WM patients with acquired VWD, as well as outcomes following therapy have not been well characterized.
Methods: We carried a retrospective study in patients with new diagnosed diagnosed WM who were evaluated at our institution, and tested for the presence of VWD. The presence of any VWD was evaluated by measuring levels of VW factor antigen (VWFAG), VW factor activity (VWFACT) and factor VIII (FVIII). Low-level VWD was diagnosed if VWFAG, VWFACT and FVIII levels were between 30% and 50%. VWD was diagnosed if VFWAG, VWFACT and FVIII were <30%. Univariate and multivariate logistic regression models were fitted to evaluate association of clinical factors and presence of any VWD. We also evaluated the effect of response to therapy on VWFAG, VWFACT and FVIII levels.
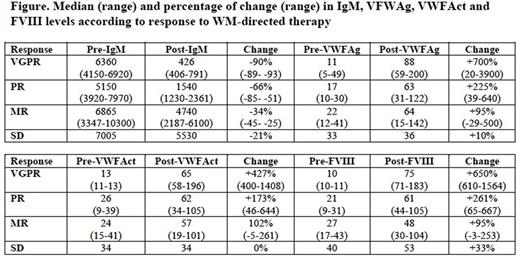
Results: A total of 320 patients with WM were tested for VWD, of whom 271 (85%) showed no evidence of deficiency, and 49 (15%) showed any VWD. Patients were tested because they provided a history of easy bruising or bleeding. Thirty patients had low-level VWD (61%) and 19 were VWD (39%). The median IgM level of patients with any VWD was 5,660 mg/dl (range 1,800-10,300 mg/dl) and 2270 mg/dl (95% CI 25-11,000 mg/dl) in patients without VWD. Patients with any VWD were more likely to have IgM levels 3,000-5,999 mg/dl and 6,000+ mg/dl (47% vs. 31%, and 45% vs. 6%, respectively; p<0.001) and less likely to have white blood cell count (WBC) >6 K/uL (29% vs. 50%; p=0.006) than patients without VWD. There were no differences in age, sex, hemoglobin levels, platelet count and bone marrow involvement between WM patients with any and without VWD. In the multivariate regression analyses, patients with IgM levels 3,000-5,999 mg/dl and 6,000+ mg/dl had OR 11.1 (95% CI 3.7-33.3; p<0.001) and OR 48.7 (95% CI 14.7-160.8; p<0.001), respectively, of having any VWD. WBC was not associated with presence of any VWD (p=0.34). In the subset of patients who had genomic testing performed (n=125), patients with any VWD were more likely to carry CXCR4 mutations (77% vs. 37%, p<0.001) than patients without VWD. There were no clinical or genomic differences between patients with low level VWD and actual VWD. Of 18 patients with any VWD who received therapy for WM, 6 patients (33%) received proteasome inhibitors + rituximab, 5 (28%) received alkylators + rituximab, 5 (28%) received ibrutinib and 2 (11%) received rituximab alone. Three patients (17%) achieved very good partial response (VGPR), 6 (33%) partial response, 8 (44%) minor response and 1 (11%) stable disease. At the moment of best response, the median IgM level had decreased from 6241 mg/dl to 2274 mg/dl, the median VWFAG level had increased from 21% to 64%, the median level VWFACT had increased from 23% to 58% and the median FVIII had increased from 21% to 57% (p<0.001 for all comparisons). Before therapy, 6 patients (33%) had low-level VWD and 12 (67%) had VWD. After therapy, 14 patients (78%) did not have VWD, 4 (22%) had low-level VWD and no patients had VWD. The depth of response to therapy (change in IgM) correlated with the percentage of change in VFWAG, VWFACT and FVIII (see Figure).
Conclusion: Patients with WM can present with acquired VWD, which seems to strongly correlate with high serum IgM levels. VWD improves and in most cases resolves with response to WM therapy. The depth of response to therapy correlates with the degree of improvement in VWD.
Castillo: Pharmacyclics: Consultancy, Research Funding; Janssen: Consultancy, Research Funding; Millennium: Research Funding; Abbvie: Research Funding. Treon: Pharmacyclics: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal